Mitral Regurgitation (MR) accounts for the vast majority of all mitral valve diseases.1 It has a prevalence of approximately 2% in the general population and is more common in the elderly population.3 Approximately 10% of people over the age of 70 have clinically meaningful MR.5
If left untreated, MR can lead to Heart Failure (HF), or deterioration of pre-existing HF, resulting in an increased number of hospital admissions and a substantial cost burden to health systems.6,8

MITRAL VALVE DISEASE
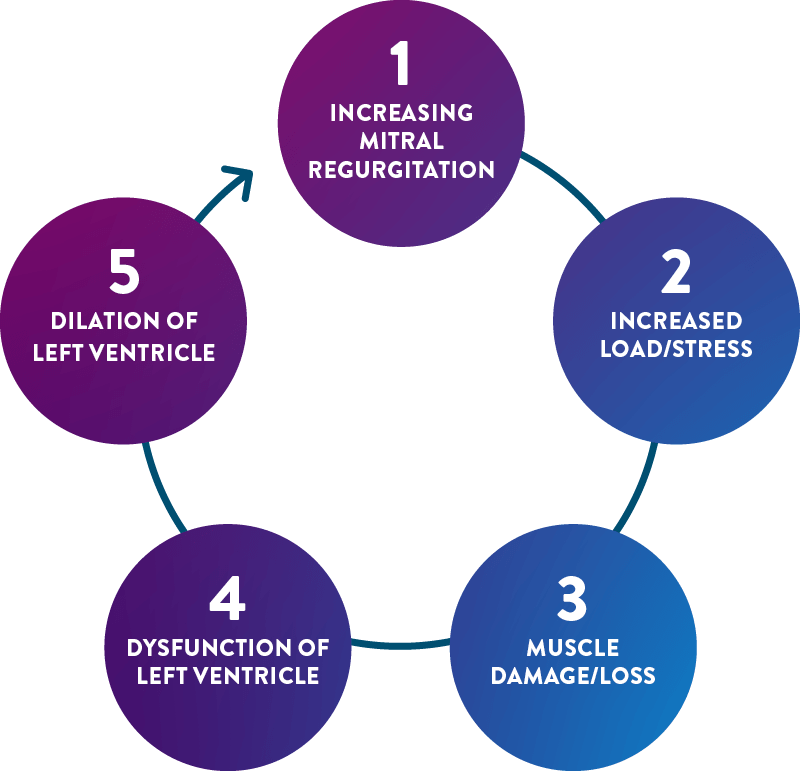
Mitral Regurgitation (MR) occurs when the mitral valve leaflets fail to properly close during ventricular contraction (systole) so blood flows back into the left atrium, leading to inefficient pumping of blood around the body.9,18
Primary (e.g. degenerative or organic) Mitral Regurgitation (PMR) is caused by abnormalities in one or more components of the mitral valve architecture, such as the leaflets, chordae, or papillary muscles.10,11
Secondary Mitral Regurgitation (SMR), also referred to as Functional Mitral Regurgitation (FMR), occurs as a result of left ventricle dysfunction, which is typically caused by ischaemic heart disease or dilated cardiomyopathy. In SMR, the mitral valve is in itself normal.10,11
LEARN MORE:
Two Types of Mitral Regurgitation
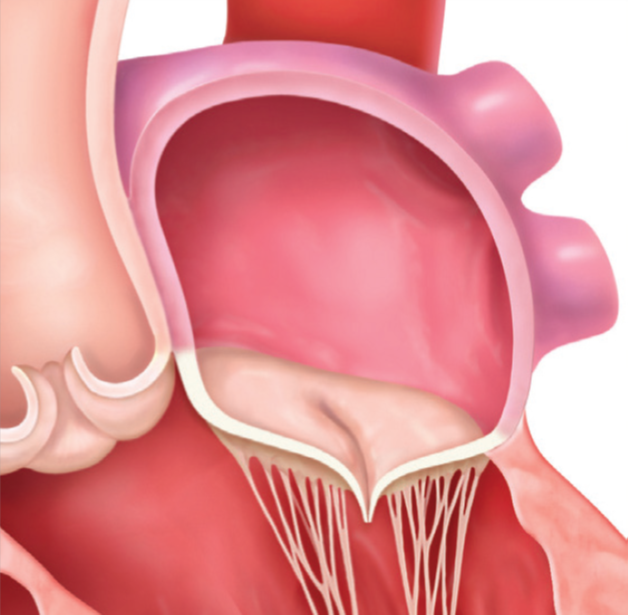
Normal
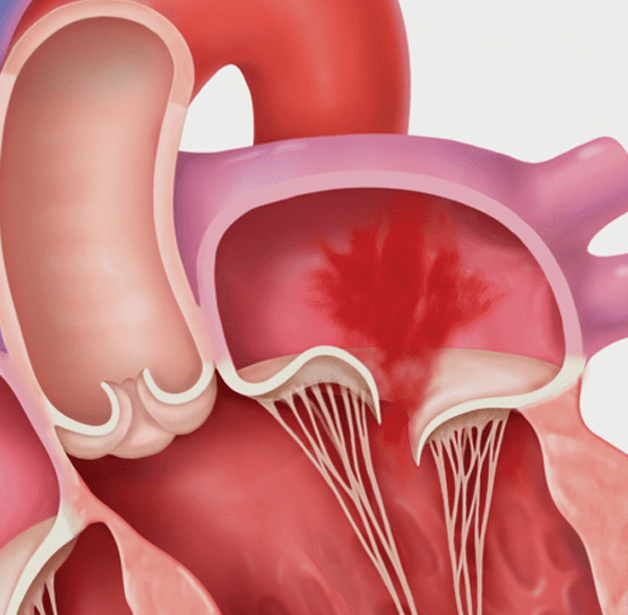
Primary MR

Secondary MR
TREATMENT OF MR
Treatment of MR is guided by the disease classification (primary/secondary) and severity. In SMR the approach to treatment is also guided by the nature of the patient’s underlying heart disease. The best treatment approach for a given patient and their condition (whether it be PMR or SMR) is determined by a Multidisciplinary Heart Team (MDT).16 Treatment options for MR include medical management, surgical repair or replacement, and Transcatheter Mitral Valve repair (TMVr) or Replacement (TMVR). Transcatheter Edge-to-Edge Repair (TEER) is a minimally invasive TMVr option.
TV
TV
HUB
- Lung B, Baron G, Butchart EG, et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J.
2003;24(13):1231–43. doi.org/10.1016/S0195-668X(03)00201-X. - De Bonis M, Al-Attar N, Antunes M, et al. Surgical and interventional management of mitral valve regurgitation: a position statement from the European Society of Cardiology
Working Groups on Cardiovascular Surgery and Valvular Heart Disease. Eur Heart J. 2016;37(2):133–9. doi.org/10.1093/eurheartj/ehv322. - Cahill TJ, Prothero A, Wilson J, et al. Community prevalence, mechanisms and outcome of mitral or tricuspid regurgitation. Heart. 2021;107(12):1003–9.
dx.doi.org/10.1136/heartjnl-2020-318482. - Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. The Lancet.
2012;380(9836):37–43. doi.org/10.1016/S0140-6736(12)60240-2. - Singh JP, Evans JC, Levy D, et al. Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (the Framingham Heart Study). Am J Cardiol.
1999;83(6):897–902. doi.org/10.1016/S0002-9149(98)01064-9. - Alegria-Barrero E, Chan PH, Paulo M, et al. Edge-to-edge percutaneous repair of severe mitral regurgitation–state-of-the-art for Mitraclip™ implantation. Circ J.
2012;76(4):801–8. doi.org/10.1253/circj.CJ-11-1462. - Healthcare Commission. Pushing the boundaries. Improving services for people with heart failure. 2007. Available at: webarchive.nationalarchives.gov.uk/ukgwa/20081006104707/
www.cqc.org.uk/_db/_documents/Pushing_the_boundaries_Improving_services_for_patients_with_heart_failure_200707020413.pdf (last accessed: 23 March 2023). - Braunschweig F, Cowie MR, Auricchio A. What are the costs of heart failure? Europace. 2011;13 Suppl 2:ii13–7. doi.org/10.1093/europace/eur081.
- Pedrazzini GB, Faletra F, Vassalli G, et al. Mitral regurgitation. Swiss medical weekly. 2010;140(3–4):36–43. doi.org/10.4414/smw.2010.12893.
- Mayo Clinic. Mitral valve regurgitation. 2019. Available at: www.mayoclinic.org/diseases-conditions/mitral-valve-regurgitation/symptoms-causes/syc-20350178
(last accessed: March 2023). - Sparano DM, Ward RP. Management of asymptomatic, severe mitral regurgitation. Current treatment options in cardiovascular medicine. 2012;14(6):575-83.
- Cioffi G, Tarantini L, De Feo S, et al. Functional mitral regurgitation predicts 1-year mortality in elderly patients with systolic chronic heart failure. Euro J Heart Fail.
2005;7(7):1112–7. doi.org/10.1016/j.ejheart.2005.01.016. - Enriquez-Sarano M, Avierinos J-F, Messika-Zeitoun D, et al. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med.
2005;352(9):875–83. doi.org/10.1056/NEJMoa041451. - Grigioni F, Tribouilloy C, Avierinos J-F, et al. Outcomes in mitral regurgitation due to flail leaflets a multicenter European study. JACC Cardiovascular Imaging.
2008;1(2):133–41. doi.org/10.1016/j.jcmg.2007.12.005. - McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the
diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA)
of the ESC. Eur Heart J. 2021;42(36):3599–3726. doi.org/10.1093/eurheartj/ehab368. - Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of
valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Euro Heart J. 2022;43(7):561–632.
doi.org/10.1093/eurheartj/ehab395. - Gaasch WH, Meyer TE. Left ventricular response to mitral regurgitation: implications for management. Circulation. 2008;118(22):2298–2303.
doi.org/10.1161/CIRCULATIONAHA.107.755942. - National Health Service. Mitral valve problems. 2020. Available at: www.nhs.uk/conditions/mitral-valve-problems(last accessed: March 2023).
- American Heart Association. Problem: Mitral Valve Regurgitation. 2016. Available at: www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valveproblems-and-causes/problem-mitral-valve-regurgitation (last accessed: March 2023).
- Spieker M, Kelm M, Westenfeld R. Moderne Diagnostik der Mitral- und Trikuspidalklappe – was ist wirklich notwendig? Aktuelle Kardiologie. 2017;6:265–70.
doi.org/10.1055/s-0043-115534. - Young A, Feldman T. Percutaneous mitral valve repair. Curr Cardiol Rep. 2014;16(1):443. doi.org/10.1007/s11886-013-0443-6.
- Otto CM, Nishimura RA, Bonow RO, 3 authors, et al.. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary:
A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;143(5):e35–e71.
doi.org/10.1161/CIR.0000000000000932. - Ling LH, Enriquez-Sarano M, Seward JB, et al. Clinical outcome of mitral regurgitation due to flail leaflet. N Engl J Med. 1996;335(19):1417-1423.
doi.org/10.1056/NEJM199611073351902. - Mirabel M, Iung B, Baron G, et al. What are the characteristics of patients with severe, symptomatic, mitral regurgitation who are denied surgery? Eur Heart J.
2007;28(11):1358–65. doi.org/10.1093/eurheartj/ehm001. - Nielsen SL. Current status of transcatheter mitral valve repair therapies - From surgical concepts towards future directions. Scand Cardiovasc J. 2016;50(5-6):367-376. doi.org/10.1080/14017431.2016.1248482
- Asgar AW, Mack MJ, Stone GW. Secondary mitral regurgitation in heart failure: pathophysiology, prognosis, and therapeutic considerations. J Am Coll Cardiol. 2015;65(12):1231–1248. doi.org/10.1016/j.jacc.2015.02.009
- Iung B, Baron G, Tornos P, et al. Valvular heart disease in the community: a European experience. Curr Probl Cardiol. 2007;32(11):609-661. doi.org/10.1016/j.cpcardiol.2007.07.002
- Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895–e1032. doi.org/10.1161/CIR.0000000000001063
- Coats AJS, Anker SD, Baumbach A, Alfieri O, von Bardeleben RS, Bauersachs J, et al. The management of secondary mitral regurgitation in patients with heart failure: a joint position statement from the Heart Failure Association (HFA), European Association of Cardiovascular Imaging (EACVI), European Heart Rhythm Association (EHRA), and European Association of Percutaneous Cardiovascular Interventions (EAPCI) of the ESC. Euro Heart J. 2021;42(13):1254–1269. doi.org/10.1093/eurheartj/ehab086
- European Heart Journal, Volume 46, Issue 44, 21 November 2025, Pages 4635–4736, doi.org/10.1093/eurheartj/ehaf194