Aortic Stenosis (AS) is the most common primary valve disease leading to surgery or catheter intervention in Europe and North America.1 It is present in approximately 2% of the general population with a rising prevalence in the elderly (up to 6% in patients above 85 years old).2-4
Symptomatic AS has significant effects on a patient’s health and quality of life5,6 and many will have cardiovascular and other comorbidities, for example, other valvular diseases, diabetes mellitus, hypertension and peripheral vascular disease.7-11
Aortic Stenosis is the narrowing of the aortic orifice, typically as a result of degeneration and calcification of the valve leaflets.2
A normal aortic valve has an orifice of 3 to 4 cm.2,12 Narrowing of the valve becomes hemodynamically significant when the valve area is reduced to about 1 cm.2 AS leads to a less optimal flow of blood from the ventricle into the aorta and may result in Left Ventricle (LV) hypertrophy and decreased systemic and coronary circulation.
Anatomy of the aortic valve: types of aortic stenosis
Normal

Mild-to-Moderate Aortic Stenosis

Severe Aortic Stenosis
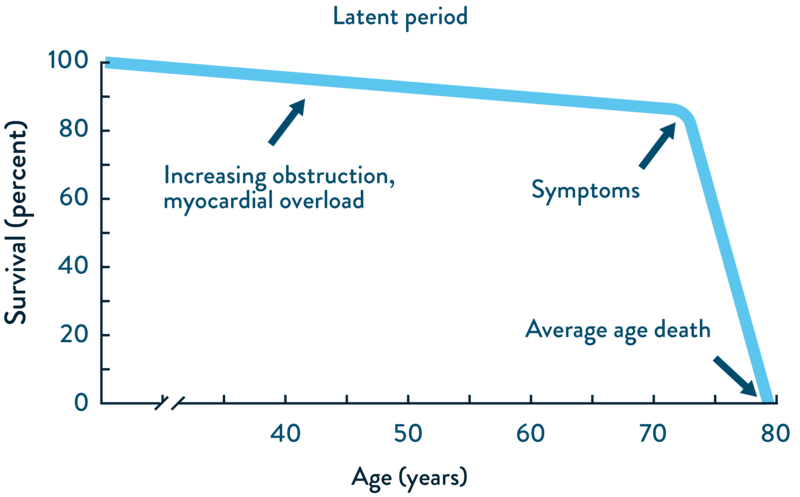
AS is a progressive disease. While patients with AS may initially be asymptomatic, further progression is typically associated with symptoms and poor prognosis.13,14 AS is associated with a significant risk of mortality, and survival is markedly reduced after the onset of symptoms.15
Natural history of AS:16
TV
TV
HUB
- Falk V, Baumgartner H, Bax JJ et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur J Cardiothorac Surg. 2017;52(4):616–664. doi.org/10.1093/ejcts/ezx324.
- Lindroos M, Kupari M, Heikkilä J et al. Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J Am Coll Cardiol. 1993;21(5):1220–1225. doi.org/10.1016/0735-1097(93)90249-Z.
- Osnabrugge RLJ, Mylotte D, Head SJ et al. Aortic stenosis in the elderly: disease prevalence and number of candidates for transcatheter aortic valve replacement: a meta-analysis and modeling study. J Am Coll Cardiol. 2013;62(11):1002–1012. doi.org/10.1016/j.jacc.2013.05.015.
- d'Arcy JL, Coffey S, Loudon MA et al. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: the OxVALVE Population Cohort Study. Eur Heart J. 2016;37(47):3515–3522. doi.org/10.1093/eurheartj/ehw229.
- van Geldrop MWA, Heuvelman HJ, Kappetein AP et al. Quality of life among patients with severe aortic stenosis. Neth Heart J. 2013;21(1):21–27. doi.org/10.1007/s12471-012-0364-9.
- Oterhals K, Haaverstad R, Nordrehaug JE et al. Self-reported health status, treatment decision and survival in asymptomatic and symptomatic patients with aortic stenosis in a Western Norway population undergoing conservative treatment: a cross-sectional study with 18 months follow-up. BMJ Open. 2017;7(8):e016489. dx.doi.org/10.1136/bmjopen-2017-016489.
- Iung B, Baron G, Tornos P et al. Valvular heart disease in the community: a European experience. Curr Probl Cardiol. 2007;32(11):609–661. doi.org/10.1016/j.cpcardiol.2007.07.002.
- Faggiano P, Frattini S, Zilioli V et al. Prevalence of comorbidities and associated cardiac diseases in patients with valve aortic stenosis. Potential implications for the decision-making process. Int J Cardiol. 2012;159(2):94–99. doi.org/10.1016/j.ijcard.2011.02.026.
- Maisano F, Worthley S, Rodés-Cabau J et al. Early commercial experience from transcatheter aortic valve implantation using the Portico™ bioprosthetic valve: 30-day outcomes in the multicentre PORTICO-1 study. EuroIntervention. 2018;14(8):886–893. doi.org/10.4244/EIJ-D-18-00343.
- Reardon MJ, Van Mieghem NM, Popma JJ et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017;376(14):1321–1331. doi.org/10.1056/NEJMoa1700456.
- Leon MB, Smith CR, Mack MJ et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016;374(17):1609–1620. doi.org/10.1056/NEJMoa1514616.
- Olszowska M. Pathogenesis and pathophysiology of aortic valve stenosis in adults. Pol Arch Med Wewn. 2011;121(11):409–413. www.mp.pl/paim/issue/article/1103/.
- Czarny MJ et al. Diagnosis and management of valvular aortic stenosis. Clin Med Insights Cardiol. 2014;8(Suppl 1):15–24. doi.org/10.4137/CMC.S15716.
- Nishimura RA, Otto CM, Bonow RO et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Thorac Cardiovasc Surg. 2014;148(1):e1–e132. doi.org/10.1016/j.jtcvs.2014.05.014.
- Zakkar M, Bryan AJ, Angelini GD. Aortic stenosis: diagnosis and management. BMJ. 2016;355:i5425. doi.org/10.1136/bmj.i5425.
- Indolfi C, Bartorelli AL, Berti S et al. Updated clinical indications for transcatheter aortic valve implantation in patients with severe aortic stenosis: expert opinion of the Italian Society of Cardiology and GISE. J Cardiovasc Med (Hagerstown). 2018;19(5):197–210. doi.org/10.2459/JCM.0000000000000636.
- Grimard BH, Safford RE, Burns EL. Aortic stenosis: diagnosis and treatment. Am Fam Physician. 2016;93(5):371–378. www.aafp.org/pubs/afp/issues/2016/0301/p371.html.
- Vahanian A, Beyersdorf F, Praz F et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022;43(7):561–632. doi.org/10.1093/eurheartj/ehab395
- Kanwar A, Thaden JJ, Nkomo VT. Management of patients with aortic valve stenosis. Mayo Clin Proc. 2018;93(4):488-508. doi.org/10.1016/j.mayocp.2018.01.020.
- “Aortic Valve Stenosis - Diagnosis and Treatment - Mayo Clinic.” Aortic Valve Stenosis - Diagnosis and Treatment - Mayo Clinic, 18 August 2022, www.mayoclinic.org/diseases-conditions/aortic-stenosis/diagnosis-treatment/drc-20353145 (accessed May 2023).
- Ram E, Sternik L, Lipey A, et al. Clinical and echocardiographic outcomes after aortic valve repair in patients with bicuspid or unicuspid aortic valve. Isr Med Assoc J. 2018;20(7):423–428. www.ima.org.il/FilesUploadPublic/IMAJ/0/294/147319.pdf.
- Martín M, Lorca R, Rozado J, et al. Bicuspid aortic valve syndrome: a multidisciplinary approach for a complex entity. J Thoracic Dis. 2017;9(Suppl 6):S454–S464. doi.org/10.21037/jtd.2017.05.11.
- Généreux P, Stone GW, O'Gara PT et al. Natural history, diagnostic approaches, and therapeutic strategies for patients with asymptomatic severe aortic stenosis. J Am Coll Cardiol. 2016;67(19):2263–2288. doi.org/10.1016/j.jacc.2016.02.057.
- Lund O. Preoperative risk evaluation and stratification of long-term survival after valve replacement for aortic stenosis. Reasons for earlier operative intervention. Circulation. 1990;82(1):124–139. doi.org/10.1161/01.CIR.82.1.124.
- Nashef SA, Roques F, Sharples LD et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41(4):734–744;discussion 744–745. doi.org/10.1093/ejcts/ezs043.
- Roques F, Michel P, Goldstone AR et al. The logistic EuroSCORE. Eur Heart J. 2003;24(9):881–882. doi.org/10.1016/S0195-668X(02)00799-6.
- Roques F, Nashef SA, Michel P et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg. 1999;15(6):816–822;discussion 822–823. doi.org/10.1016/S1010-7940(99)00106-2.
- Thourani VH, Suri RM, Gunter RL et al. Contemporary real-world outcomes of surgical aortic valve replacement in 141,905 low-risk, intermediate-risk, and high-risk patients. Ann Thorac Surg. 2015;99(1):55–61. doi.org/10.1016/j.athoracsur.2014.06.050.
- Brown JM, O’Brien SM, Wu C et al. Isolated aortic valve replacement in North America comprising 108,687 patients in 10 years: changes in risks, valve types, and outcomes in the Society of Thoracic Surgeons National Database. J Thorac Cardiovasc Surg. 2009;137(1):82–90. doi.org/10.1016/j.jtcvs.2008.08.015.
- Culler SD, Cohen DJ, Brown PP et al. Trends in aortic valve replacement procedures between 2009 and 2015: has transcatheter aortic valve replacement made a difference? Ann Thorac Surg. 2018;105(4):1137–1143. doi.org/10.1016/j.athoracsur.2017.10.057.
- O'Brien SM, Shahian DM, Filardo G et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 2--isolated valve surgery. Ann Thorac Surg. 2009; 88(1 Suppl):S23–42. doi.org/10.1016/j.athoracsur.2009.05.056.
- Durko AP, Osnabrugge RL, Kappetein AP. Long-term outlook for transcatheter aortic valve replacement. Trends Cardiovasc Med. 2018;28(3):174–183. doi.org/10.1016/j.tcm.2017.08.004.
- McDonagh TA, Metra M, Adamo M et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–3726. doi.org/10.1093/eurheartj/ehab368.
- Filardo G, Hamilton C, Hamman B et al. New-onset postoperative atrial fibrillation and long-term survival after aortic valve replacement surgery. Ann Thorac Surg. 2010;90(2):474–479. doi.org/10.1016/j.athoracsur.2010.02.081.
- European Heart Journal, Volume 46, Issue 44, 21 November 2025, Pages 4635–4736, doi.org/10.1093/eurheartj/ehaf194